Is the geriatric patient a drug user or a victim?

Published Nov. 14, 2024 08:00

According to the definition, a geriatric patient is a person over the age of 60, whose body is constantly changing due to the progressive aging process of the body. As time passes, absorption weakens, gastric juice acidity and peristalsis decrease, liver metabolism slows down, kidneys function less well. These are just a few examples of the changes taking place, but everything that happens in the body can affect how we react to the drugs we take. According to statistics, 15-20% of hospitalizations of people over 65 are caused by side effects of medications. The more a patient takes them, the higher the risk of side effects.
Therapeutic chaos
Most seniors are treated by primary care doctors, but they also seek help from various specialists. They go to the doctor because a new problem has arisen that they want to solve. But they go unprepared. They usually don't tell the doctor about their chronic diseases and the medications they are taking. The doctor does not ask or asks very rarely. If he recognizes an ailment, he issues a prescription for another drug and everyone thinks the problem is solved. Are you sure? The consequence of such behavior is so-called therapeutic chaos, which leads, among other things, to seniors taking from three to more than 10 medications a day. Taking eight drugs a day is associated with a 100% occurrence of interactions [1, 2].
One more issue worth mentioning is the drug cascade. This is a concept that refers to the phenomenon of prescribing or self-incorporating new drugs. The drug cascade occurs as a result of the treatment of various conditions by specialist doctors who have not been informed of other drugs used by the patient. The number of drugs used by a senior should be reduced not only because of the possibility of interactions, but also because of improved compliance, which leads to more effective treatment.
Through the eyes of a pharmacologist
Blaming geriatric patients for drug addiction is unjustified, since most of them try to follow their doctors' instructions. Yes, there are elderly people who abuse medications, just as there are people who overeat sweets. When meeting a patient with a doctor, the former is completely defenseless. He takes on faith everything the doctor says and recommends. Most patients do not analyze the specialist's decision, because they are not familiar with medicine and do not know what drug interactions are. They do not inquire how to take the drug and what not to combine it with.
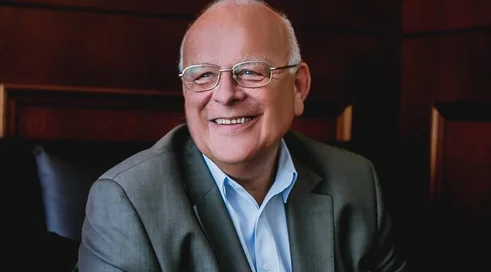
- For a geriatric patient, a professional health care professional is like St. Peter, because he gives hope for a pass to continue living, says Dr. n. pharm. Leszek Borkowski, a clinical pharmacologist at the Mazovian Bródnowski Hospital. - Hence, any carelessness or oversight we make reflects on the geriatric patient. I work as a clinical pharmacologist in a large Warsaw hospital. I deal with patients through the medications they take. As a pharmacist, I don't diagnose or determine first-line therapy. I show up when it is necessary with a multi-disease, or multi-drug patient to swap something with something, recommend a different dosage, frequency, choose medications for exacerbation of chronic renal or liver failure, suggest additional laboratory and radiological diagnostic tests, and so on.
- Every drug needs to be discussed with the patient so that they can wisely help with therapy by watching for the side effects that begin, which are trivial to deal with at the beginning in relation to later hospitalizations. If I'm doing a bad job, I won't ask the patient or his caregivers about lab results, medications taken prior to hospital admission, I won't ask about OTC drugs or dietary supplements, miracle herbs and concoctions bought at fairs and markets along with veal, eggs and white cheese. Sometimes patients don't know what drugs they are taking and inform me in a very simplistic way, describing the color of the pill or the size of the package.
- The problem could be attempted to be solved by assigning centrally in the system all drugs bought at the pharmacy by the patient, the expert continues. Maybe the National Health Service will let this data into its systems for controlling prescribing. I am often asked whether seniors are drug addicts? I answer - no. The geriatric patient is lost and poorly taken care of by me as a pharmacologist. I no longer throw out "miracle concoctions and marketing inventions from the media, the Internet" etc. from patients' cabinets because complaints were written against me. Having worked for many years in various hospitals, I am becoming more and more distanced. Now I only try to explain, convince. The patient is sometimes on my side, but his family is not always, or rather against, because, like Carnation, they know better.
Needed drug review
In April 2021, the Law on the Pharmaceutical Profession, which recognizes the pharmacy profession as a medical profession, went into effect. There are plans to implement the service, which has been dubbed drug review.
Drug review is to be a pharmaceutical service, part of pharmaceutical care. As part of such advice, the pharmacist will check whether medications taken by the patient have clinically significant interactions with each other. The pharmacist community is very much looking forward to this project, especially since the drug review pilot went very favorably. The pilot took off in early April 2022, and 75 appropriately trained pharmacists from all over Poland participated. The pilot covered 850 patients. The basic eligibility criterion was taking a minimum of 10 prescription and over-the-counter drugs.
The problem of multidrug use affects more than 600,000 patients in Poland. It is worth mentioning that already with regular use of three drugs, the risk of harmful interactions and side effects exceeds 80%. Pharmacists hope that drug review will be included in the basket of guaranteed benefits in 2024. Let's hope this happens.
By the thread to the puck
Why is drug review a very important and necessary service? First of all, because the problem of multi-disease and multi-medication is growing because we are an aging society. Seniors are taking too many medications. As we said, it's not because they are drug addicts, but because they don't have proper care.
To show what the problem is, we asked Dr. Leszek Borkowski (a clinical pharmacologist) to analyze the medications taken by a specific person. We assure you, this is a flesh-and-blood person, not invented for the purpose of this article.
- The patient, a senior citizen with multimorbidity, is taking too many preparations, those prescribed by doctors and those available over-the-counter, as well as supplements dropped off by her children to make mommy healthier, Dr. Borkowski said. - But sometimes the bigger problem in pharmacological evaluation is not the number of preparations, but the lack of check-ups associated with prescribed medications. This is hardly discussed and written about.
The medications our patient is taking are: Nebilet, Tritace, Lacipil, Atorvasterol, Devikap, Trexan, Acidum folicum, Eutyrox, Polocard Helicid, Magne B6 Forte, Litorsal senior, Hepaslimin, Melatonin, and Positivum on Saturdays and Sundays, as her grandchildren and daughter-in-law come over. Quite often various NSAID painkillers.
Nebilet - nebivolol
If there is or will be liver failure or liver dysfunction following concurrent use of methotrexate and nebilet, Nebilet becomes contraindicated for use.
Tritace - ramipril
It is recommended to take the product every day at the same time of day (the patient does not know it). For elderly patients, initial doses should be smaller and increased very slowly.
We would like to warn the patient that the occurrence of cough during the use of ACE inhibitors (Tritace) has been described. Typically, the cough is non-productive, persistent and resolves when treatment is discontinued and there is no need to step in with cough suppressants.
Lacipil - lacidipine
Store at temperatures below 30oC. In summer, we have higher temperatures in sunny apartments. Protect tablets from light and remove from blister immediately before taking. Lacipil should be used with caution in patients with hepatic impairment due to the possibility of increased hypotensive effect. Importantly - do not eat grapefruit or drink grapefruit juice. Concomitant use of lacydipine with corticosteroids may reduce its hypotensive effect. The patient uses ointments for painful joints, but she doesn't know which ones, and I'm not sure if she doesn't use ointments containing glucocorticosteroids. Nebilet, Tritace, Lacipil are classic combination therapy - old, but used quite commonly.
Atorvasterol - atorvastatin
Atorvasterol is used as an adjunct to dietary treatment to lower elevated levels of total cholesterol, LDL cholesterol, apolipoprotein B and triglycerides in adults. The patient doesn't have and hasn't been prescribed any diet, maybe she should consult a dietitian and start by changing her eating habits, just be sure to tell her. Before starting treatment with Atorvasterol, the patient should follow a standard low-cholesterol diet, which should be continued during treatment. The use of this drug is contraindicated in patients with active liver disease. Since Atorvastatin is contraindicated in patients with active liver disease or unexplained, persistently elevated serum aminotransferase activity exceeding 3 times the upper limit of normal, I understand that the patient has had serum aminotransferase levels ordered and performed prior to atorvastatin prescribing. Patients who have an increase in aminotransferase activity should be monitored until the abnormalities resolve. If there is a persistent increase in aminotransferase activity greater than three times the upper limit of normal (GGN), dose reduction or drug discontinuation is recommended.
Instruct the patient to report the onset of muscle pain, cramps or muscle weakness immediately, especially if accompanied by general malaise or fever. If these symptoms occur in a patient taking atorvastatin, creatine kinase activity should be measured. If it is significantly elevated (> 5 times GGN), the product should be discontinued.
Devikap - cholecalciferol
I hope that the dose and the decision to ordinate was due to the determination of low vitamin D3 levels. If Devikap is taken as a precaution then it should be discontinued.
Trexan - methotrexate
Rheumatic disease or psoriasis or severe psoriatic arthritis was probably the indication. The patient should be informed of all the risks associated with the therapy, and the doctor should pay special attention to the occurrence of signs of liver toxicity by performing liver function tests before starting treatment with methotrexate, and then repeating them during the course of therapy.
A senior patient taking methotrexate should undergo follow-up examinations at shorter intervals including a blood count, creatinine level, and examination of the mouth and throat to rule out mucosal lesions. Patients should be advised of the risk of pneumonia and instructed to contact their doctor immediately if they develop a persistent cough or persistent shortness of breath.
In patients with respiratory disorders, the possibility of Pneumocystis jiroveci infection should be considered. As there are renal impairment, including mild, the concomitant use of non-steroidal anti-inflammatory drugs periodically applied by the patient herself is not recommended. There is also a likelihood of increased toxicity with low doses of methotrexate, used in combination with NSAIDs. NSAIDs can cause kidney damage.
Patients are warned that excessive consumption of caffeinated or theophylline-containing beverages (coffee, caffeinated sodas, black tea) should be avoided during methotrexate treatment, as the effectiveness of methotrexate may be reduced.
Folic acid (acidum folicum)
It is advisable to check vitamin B12 levels before starting folic acid supplementation, especially in adults over the age of 50, as taking folic acid may mask vitamin B12 deficiency. Its addition to Trexan is warranted.
Euthyrox - levothyroxine
It is recommended to determine the individual daily dose on the basis of laboratory results and clinical assessment. Take a single daily dose in the morning, on an empty stomach, half an hour before breakfast, preferably with a small amount of liquid, such as half a glass of water. This is an important but not always followed rule for taking Euthyrox.
Polocard - acetylsalicylic acid
The 2022 published position statement of US experts on the use of acetylsalicylic acid in the prevention of cardiovascular disease does not recommend that people > 60 years old take it for primary prevention of cardiovascular disease. It inhibits platelet function, thereby increasing the risk of bleeding outside the gastrointestinal tract. Bleeding risks can be trivial, but also life-threatening, including intracranial hemorrhagic strokes. I believe that the preventive use of acetylsalicylic acid in the prevention of cardiovascular disease in some patients is questionable in terms of bleeding risk.
Polcard reduces the antihypertensive effect of Tritace, meaning the two drugs should not be used together. Note: Polcard is contraindicated for concomitant use with methotrexate (Trexan).
Helicid - omeprazole
Omeprazole, like all drugs that inhibit gastric acid secretion, may reduce the absorption of vitamin B12 (cyanocobalamin) due to hypo- or achlorhydria. This should be taken into account in patients with reduced body reserves or with risk factors that favor reduced vitamin B12 absorption during long-term treatment. If taken for poor indications or as a preventive measure, it should be discontinued.
Magne B6 Forte - magnesium and pyridoxine (vitamin B6)
Particular caution should be exercised in patients with moderate renal insufficiency due to the risk of high blood magnesium levels. Without determining the level of magnesium and pyridoxine deficiency, Magne B6 Forte is eligible for withdrawal.
Summarizing his assessment of the patient's use of multiple preparations, Leszek Borkowski suggests discontinuing: Hepaslimin, Litorsal Senior, Melatonin, Positivum, Polocard. Atorvasterol, Devikap, Helicid should be taken after diagnostic tests that confirm the need. It seems reasonable to take only medications such as Nebilet, Tritace, Lacipil, Trexan, Acidum folicum.
From this cursory review of pharmacology, it is clear that in a patient who was taking 19 different medications, the list can be limited to 5 preparations!
Returning to the drug review pilot for a moment, it is worth implementing it as soon as possible so that the described situations are as few as possible. Let's hope that this will be the case.
Footnotes:
- A. Borzym, Principles of pharmacotherapy in the elderly.
- D. Ksiądzyna, A. Szeląg, Specificity of pharmacotherapy of elderly patients.